Background: Follicular lymphoma (FL) is the most common subtype of indolent non-Hodgkin lymphoma (NHL). Although most patients with FL respond well to first-line therapy, they will inevitably relapse, and the subsequent course is often characterized by a pattern of recurrent relapses with progressively shorter intervals between treatment lines. Moreover, the use of multiple consecutive therapies often leads to refractory disease with severely limited treatment options, demonstrating the need for new therapies for this patient population. Currently approved phosphoinositide 3-kinase (PI3K) inhibitors are often poorly tolerated. Parsaclisib, a potent, highly-selective, next-generation PI3Kδ inhibitor, has shown promising activity in patients with previously treated B-cell malignancies. Here, we report preliminary results of CITADEL-203 (NCT03126019), a multicenter, open-label phase 2 study of parsaclisib in relapsed or refractory (R/R) FL.
Methods: Key eligibility included, age ≥18 years, histologically confirmed R/R FL grade 1, 2, or 3a, ≥2 prior systemic therapies, Eastern Cooperative Oncology Group performance status (ECOG PS) ≤2, and ineligible for hematopoietic stem cell transplantation (HSCT). Patients were allocated to receive parsaclisib 20 mg once daily (QD) for 8 weeks followed by either 20 mg once weekly (weekly-dosing group [WG]) or 2.5 mg QD (daily-dosing group [DG]). Prophylaxis for Pneumocystis jirovecii pneumonia (PJP) was required. Objective response rate (ORR) was the primary endpoint; complete response rate (CRR), duration of response (DOR), progression-free survival (PFS), overall survival (OS), and safety and tolerability were secondary endpoints. All radiology-based endpoints were based on independent review.
Results: From March 2018 to 17January 2020 (data cut-off), 106 patients (WG, n = 22; DG, n = 84) were treated. Enrollment is ongoing (target: 120 patients). At cut-off, 39 (37%) patients had discontinued treatment, including 25 (24%) for disease progression. The median exposure (range) was 5.3 months (0.5-18.1). The median age was 67 years, and 54% of the patients were men. The median time since initial diagnosis was 6 years. At enrollment, most patients (92%) had an ECOG PS ≤1, and 43% had a Follicular Lymphoma International Prognostic Index score ≥3 (high risk). The median (range) number of prior systemic therapies was 2 (1−8); 20% of the patients had prior HSCT; 47% were refractory to and 41% had relapsed from their most recent therapy.
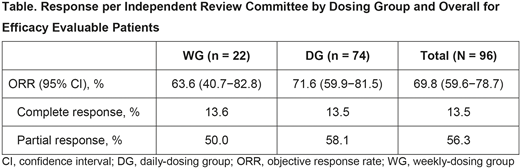
At the data cut-off, 96 patients were evaluable for response, including 74 in DG (Table). The ORR and CRR were 69.8% (95% confidence interval [CI]: 59.6−78.7) and 13.5% respectively, in all evaluable patients, and 71.6% (95% CI: 59.9% - 81.5%) and 13.5%, respectively, in DG. The median time to response was 8 weeks. The median DOR (95% CI) was not reached among responders overall (9.2 months−not estimable) and those in DG (7.4 months−not estimable). The median PFS (95% CI) was 15.8 months (11.3−15.8) overall and 15.8 months (11.0−15.8) in DG. The median follow-up (range) for this population was 10.2 months (1.9−22.2) overall and 9.5 months (1.9−21.1) in DG.
Among the 106 patients evaluable for safety, the most common treatment-emergent adverse events (TEAE) were diarrhea (27.4% of patients), nausea (22.6%), cough (18.9%), and fatigue (15.1%). The most common TEAEs grade ≥3 were diarrhea (9.4% of patients), neutropenia (6.6%), and colitis (3.8%). TEAEs leading to dose interruption or dose reduction occurred in 39.6% and 9.4% of patients, respectively. TEAEs leading to treatment discontinuation occurred in 16% of patients. Serious TEAEs observed in ≥2 patients included diarrhea (5.7% of patients), colitis (3.8%), and pleural effusion (1.9%). There were no fatal TEAEs. TEAEs of clinical interest included rash (12.3% of patients), exfoliative dermatitis (1.9%), pneumonia (0.9%), and PJP (0.9%). New or worsening grade ≥3 laboratory test values of clinical interest included increase in alanine/aspartate amino transferase (0.9%/0% of patients), and decrease in neutrophil count (8.5%), platelet count (0%), and hemoglobin (1.9%).
Conclusion: Parsaclisib demonstrated a high rate of rapid and durable response, and had an acceptable safety profile and was generally well tolerated. These results demonstrate a favorable benefit-risk profile in R/R FL. Updated data will be presented.
Lynch:Morphosys: Consultancy; Takeda: Research Funding; Incyte: Research Funding; TG therapeutics: Research Funding; Rhizen: Research Funding; Bayer: Research Funding; Juno: Research Funding; Cyteir: Research Funding; Genentech: Research Funding. Paneesha:Bristol-Myers Squibb: Honoraria; Celgene: Honoraria; Gilead: Honoraria; Janssen: Honoraria; AbbVie: Honoraria. Avigdor:Takeda, Gilead, Pfizer: Consultancy, Honoraria; Janssen, BMS: Research Funding. McKinney:Verastem: Consultancy; Pharmacyclics: Consultancy; Kite/Gilead: Honoraria, Speakers Bureau; Beigene: Research Funding; Celgene: Consultancy, Research Funding; Genentech: Consultancy, Honoraria, Research Funding; Incyte: Research Funding; Molecular Templates: Consultancy, Research Funding; Nordic Nanovector: Research Funding; Novartis: Research Funding; BTG: Consultancy. Wahlin:Gilead Sciences: Research Funding; Roche: Consultancy, Research Funding. Belada:Roche: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Research Funding; Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; Gilead: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Research Funding; Celgene: Research Funding; Takeda: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Travel expenses, Research Funding. Canales:Celgene, Gilead, iQone, Janssen, Karyopharm, Novartis, F. Hoffmann-La Roche, Sandoz: Honoraria; Janssen, F. Hoffmann-La Roche, Sandoz, Takeda: Speakers Bureau. Cunningham:Bayer: Research Funding; OVIBIO: Membership on an entity's Board of Directors or advisory committees; Amgen: Research Funding; Lilly: Research Funding; Janssen: Research Funding; Clovis Oncology: Research Funding; Celgene: Research Funding; MedImmune: Research Funding; Merck: Research Funding; Merrimack: Research Funding; Sanofi: Research Funding; AstraZeneca: Research Funding; 4SC: Research Funding. Morley:Kite: Honoraria; Janssen: Honoraria; Abbvie: Other: Conference Support; Takeda: Other: Conference Support; Roche: Other: Conference Support; Advisory board. Zheng:Incyte: Current Employment, Current equity holder in publicly-traded company. DeMarini:Incyte Corporation: Current Employment, Current equity holder in publicly-traded company. Jiang:Incyte Corporation: Current Employment, Current equity holder in publicly-traded company. Trněný:1st Faculty of Medicine, Charles University, General Hospital in Prague: Current Employment; Incyte: Consultancy, Honoraria; AbbVie: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); Amgen: Consultancy, Honoraria; Takeda: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); MorphoSys: Consultancy, Honoraria; Gilead Sciences: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); Janssen: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company); Roche: Consultancy, Honoraria, Other: TRAVEL, ACCOMMODATIONS, EXPENSES (paid by any for-profit health care company), Research Funding; Bristol Meyers Squibb: Consultancy, Honoraria, Other: TRAVEL, ACCOMODATIONS, EXPENSES (paid by any for-profit health care company); Celgene: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal